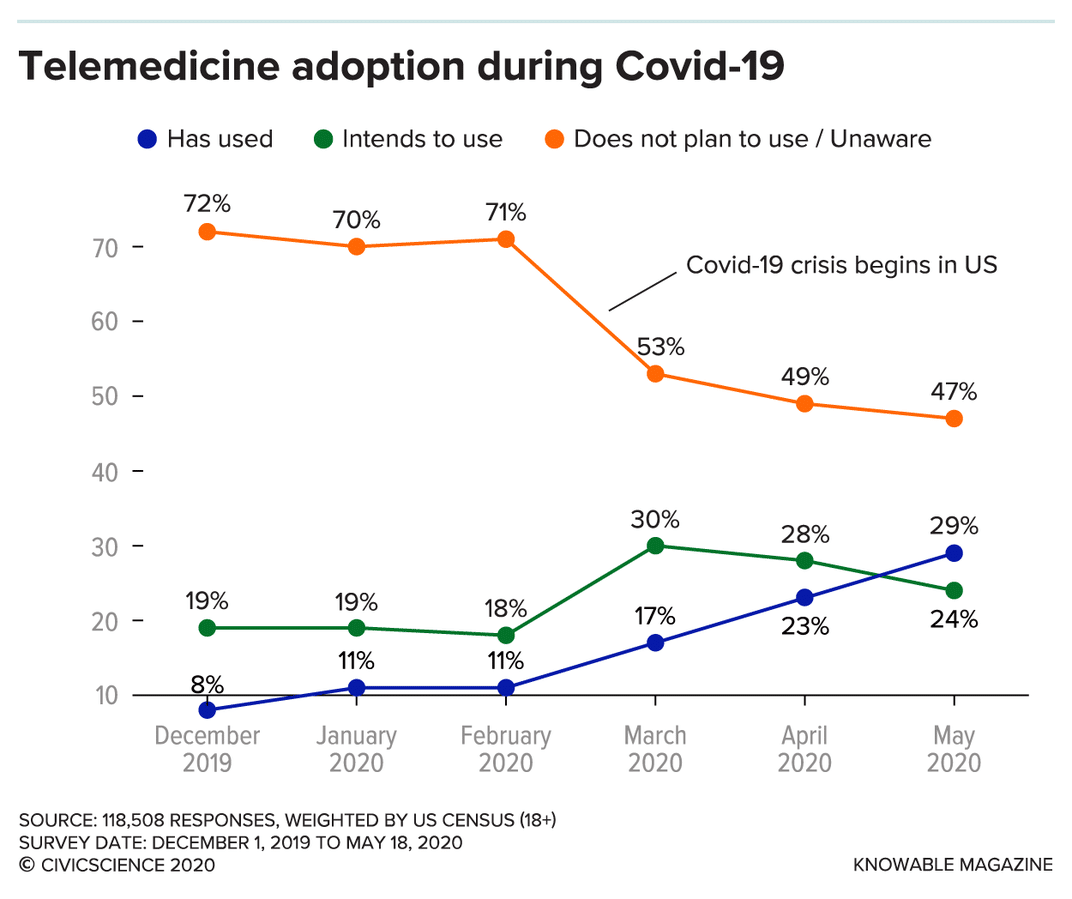
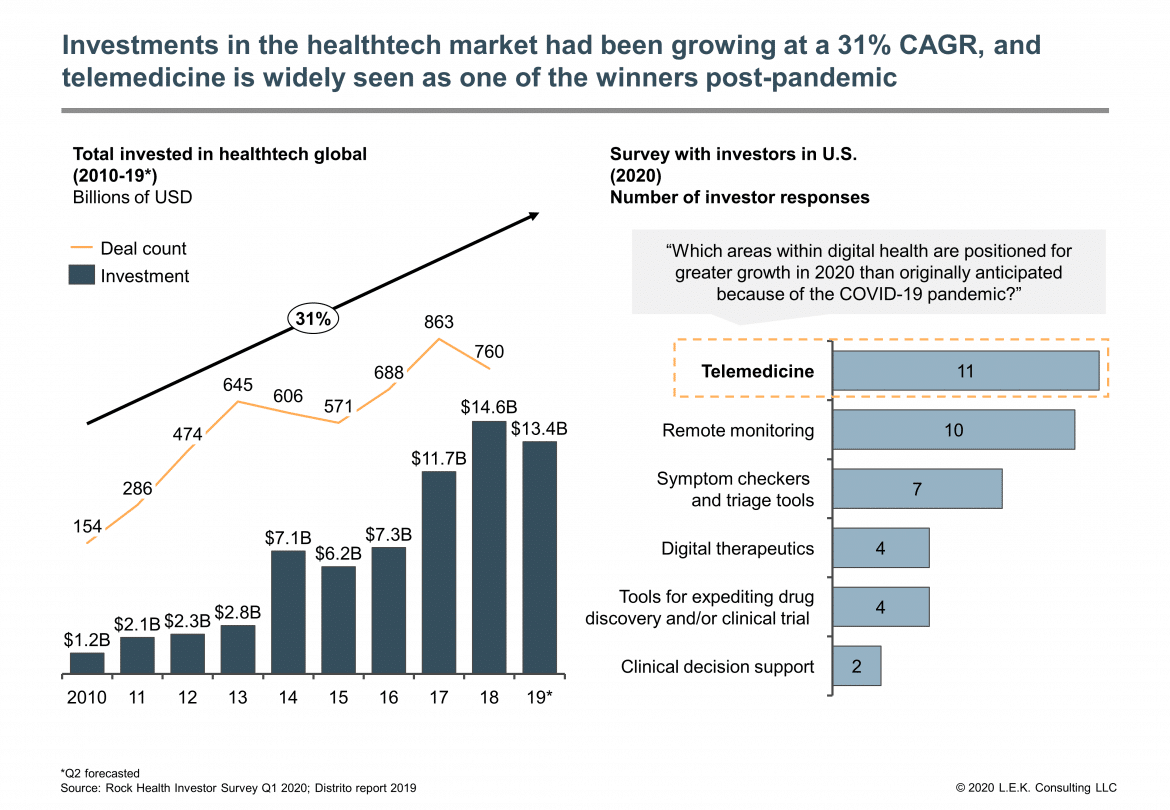
Covid-19 has forced the world into using telehealth more than it ever has before. It has been a growing industry for some time, and we should now expect to see increased adoption and development even after the pandemic is resolved.
The main area of telehealth that has come into its own during the pandemic is telemedicine, with huge amounts of appointments being moved online or to phone calls. This is something that may well continue as users realise the convenience of it, and GP practices and other healthcare professionals will have the technology readily available. There’s also an increase in cloud phone systems being used in hospitals, avoiding members of different departments having to risk infection by physically going to speak to specialists in other buildings.
State of Healthcare Today
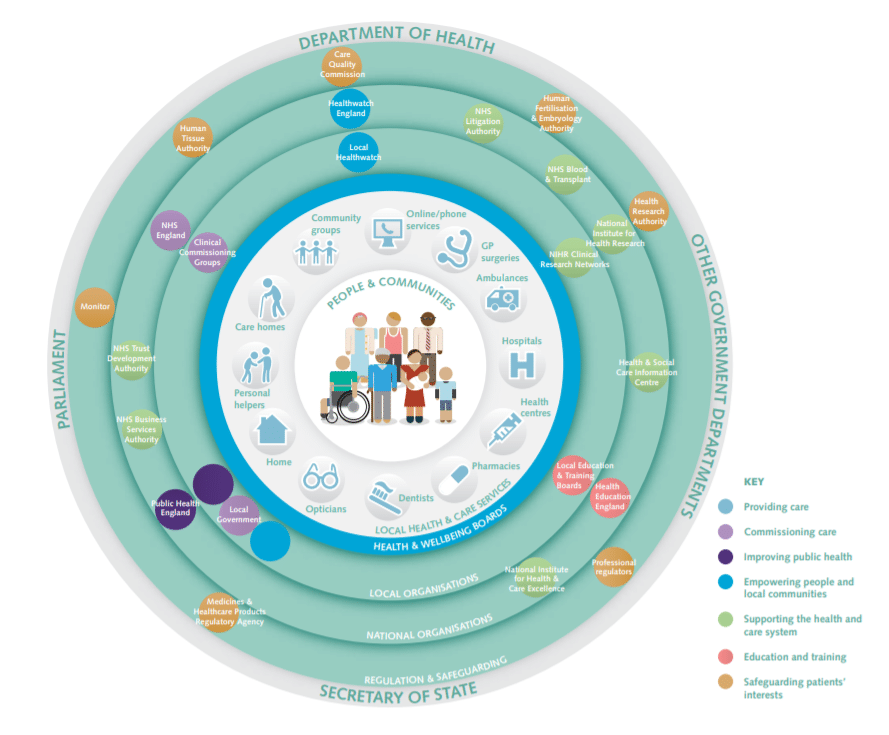
Most healthcare in the UK is provided by the NHS. In fact, they deal with over 1 million patients every 36 hours (source). Most of the publics’ contact with the health system comes from face-to-face interactions with primary care providers. This includes GPs (general practitioners), as well as dentists, opticians, and pharmacists. There are also accident and emergency departments for urgent medical care as well as walk-in centres. There is some limited use of telemedicine here, too, with the NHS 111 phone service. This is a service that can help triage a concern in real-time, and provide health information as well as send a patient to the correct provider. However, it’s ill-suited for follow-ups and is mostly designed as a point of initial contact. It’s also unable to assist with physical assessments such as taking blood pressure or visually assessing a skin condition.
Despite this – and the UK has one of the best performing healthcare systems in the world – it often lags behind when it comes to telemedicine services. Dr. Bayju Thakar, co-founder and former CEO of Doctor Care Anywhere told Doctorpreneurs that when he started the app in 2012, “the US was considerably further ahead” and that “it still is, though a lot of that has to do with scale, the structure of the healthcare system, and the incentives available.”
He noted that many of the issues with the NHS come from it dealing with a “huge array of struggles”, but is optimistic about the progress being made, saying “over the past 3 or 4 years there has been more and more dialogue with businesses like ours.”
In an interview with CNBC, Dr. Mandip Thiara, a Watford-based family doctor stated that he’s found within the NHS that “everything is slow”, and that there are “all sorts of hoops to jump through in terms of funding.” The NHS budget, according to The King’s Fund, does continue to grow but at a much slower rate than previously. The long-term average is around 3.7% a year, and the last ten years only showing 1.4% growth. With the majority of this budget going to day-to-day spending on patient care, it leaves a reduced amount available for maintaining and improving infrastructure – and that includes IT.
It’s not all bad news! For all these budgetary setbacks, there are innovative things occurring. The NHS recently announced a partnership between their digital transformation unit (NHSX) and a wearable tech company (Huma) for a trial monitoring patients’ vital signs rather than relying on a manual follow-up. These vital signs include temperature, heart rate, and blood oxygen saturation – in near real-time to help with the study of the coronavirus and its effects.
Tara Donnelly, NHSX’s chief digital officer, said of the trial “The clinical team is finding it helps give them very rapid feedback on their patients and they are able to keep an eye on a number of people at a glance, which is working much better for them than the previous system which relied on phone calls.”
In general, healthcare throughout the UK is of a good standard – the Care Quality Commission note that whilst there are flaws, it’s generally good quality and is improving slightly. However, one of the main problems it notes is a lack of access to care, particularly prevalent with children and those with mental health problems or learning disabilities.
In their State of Care report, they state “There are consequences, knock-on effects and extra pressures when people cannot easily access the care they need. In the 2019 GP Patient Survey, almost 1 in 8 people who did not make the appointment offered to them went to an emergency department instead.”
They also point out the positive impact that technology is having, saying that they have seen “a range of technologies being used to deliver care in more effective ways and to help people get a better experience of care.” Whilst limited to locations with strong management, it can make “care more person-centered.” They go on to say that they’ve also seen “some positive examples of technology being used to improve the experience of people with protected equality characteristics”, but add that this is not the norm.
The above focuses on the NHS, but there are other healthcare practitioners in the UK. Often, these private practices don’t have the same budgetary limitations, but they are much harder to access due to cost. This private care can either be accessed through health insurance – though unlike the United States, which has programs like Medicare and Medicaid, this insurance is solely covered by the individual or their employer – or paying at the point of service.
Such private care providers often need to have some level of integration or access to the NHS, especially when it comes to accessing medical records. Many will have their own doctors’ offices for in-person visits but there is occasionally overlap, especially with organisations like GP Care who handle both self-funded and NHS patients.
What is The State of Telemedicine Today?
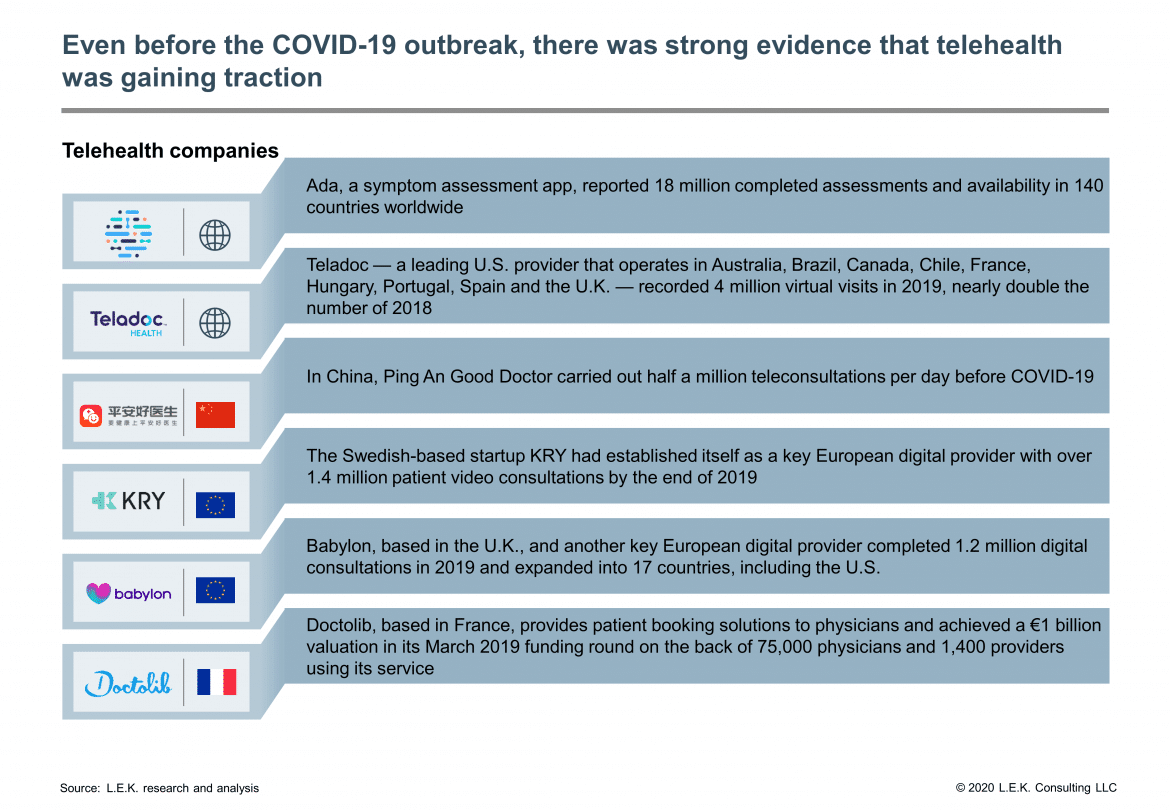
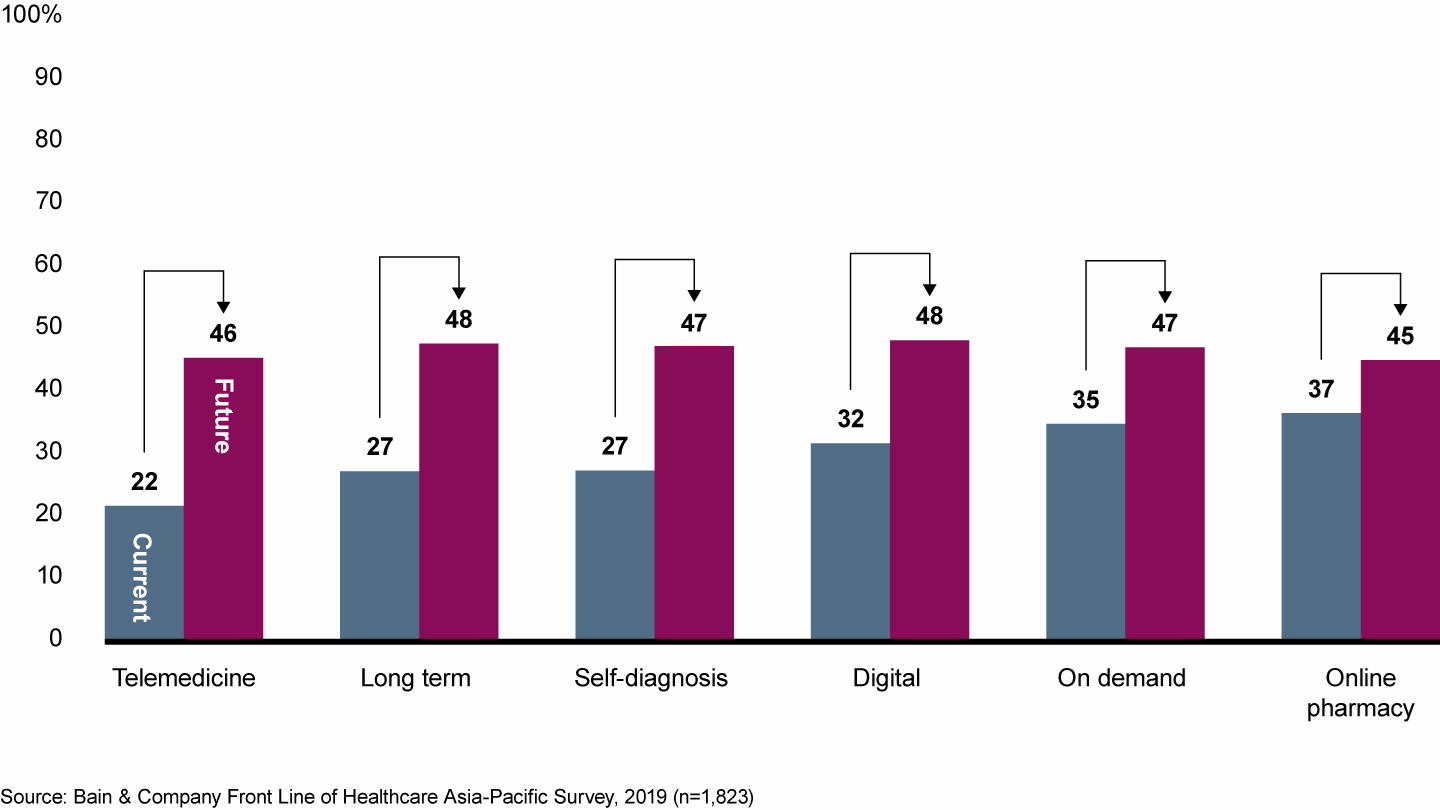
As mentioned above, there is some investment in telemedicine, but it’s limited in scope within the NHS. However, private companies are making great strides and adoption rates are increasing globally. Looking at Asia-Pacific countries, we can see that nearly 50% of respondents would use telehealth services in the next five years. This figure jumps to 91% of those services are covered by an employer or insurance.
We see similar results in the US. Joe Smith, a cardiologist who has written about telemedicine for the Annual Review of Biomedical Engineering, said of these results “I don’t think we go back…people are now seeing that they can get their health care in the safety and comfort of their own home.”
And again, similar results follow on in the UK. The former chair of the U.K.’s Royal College of General Practitioners, Dr. Clare Gerada, currently works across two practices in London. She is also co-founder of eConsult, which is an online health system that was set up by the Hurley Group (her NHS partnership). She told CNBC that she now only sees her patients face-to-face “very occasionally”, and that “about 99% or more of our care of patients has moved digitally or remotely onto the telephone…it has transformed.”
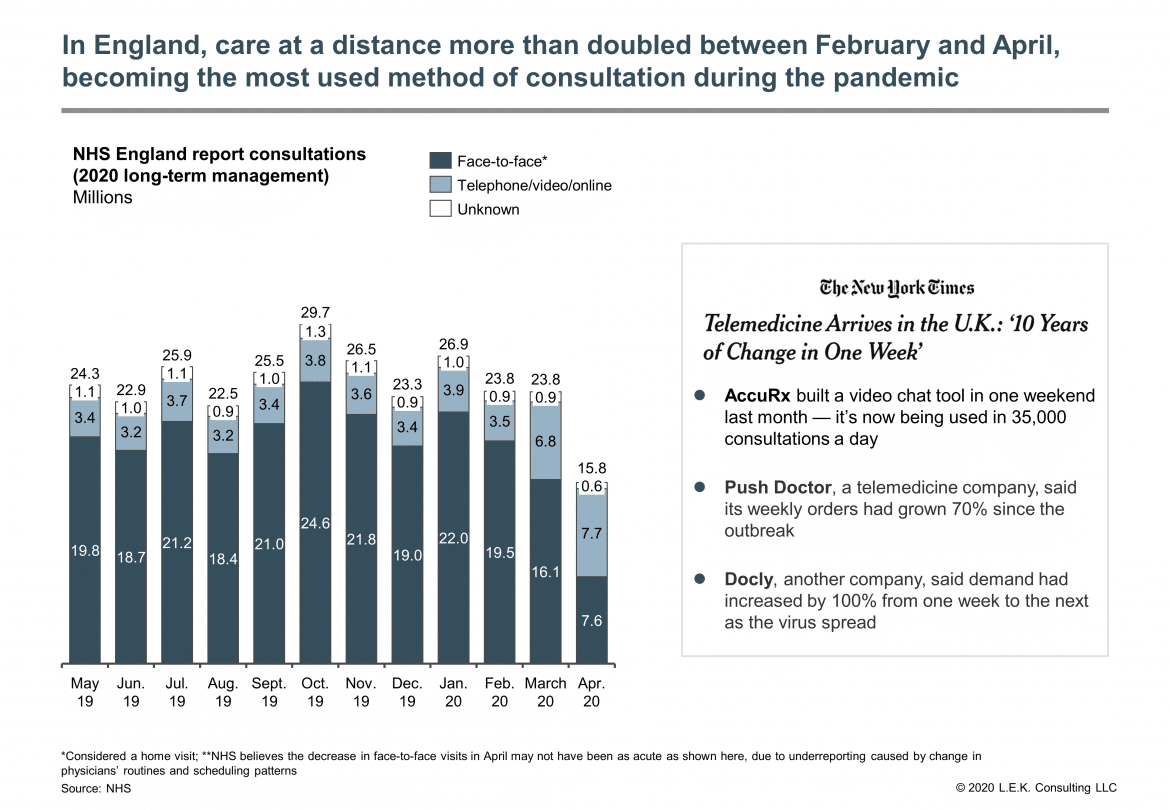
The use of eConsult has increased dramatically since coronavirus hit the UK. Two years ago, it managed around 300 consultations a month. That’s now increasing to nearly 12,000 a day or 360,000 a month – meaning they do 40 times more virtual visits in a day than they used to in an entire month.
Other companies have made great strides in the pandemic, too. Ada Health is a symptom checker, providing guidance based on data inputted by the user. It has a medical library, which is where it’s health information comes from. The benefits of telemedicine of this type have become abundantly apparent of late.
Speaking to Healthcare IT News, Dr. Claire Novorol, Ada Health’s co-founder and chief medical officer, said that they “modelled Covid-19 in [their] knowledge base so that it was one of the conditions that would be considered”. They quickly noticed many people searching specifically for COVID and decided to go a step further, building a new app to screen for coronavirus.
Dr. Novorol’s reasoning? “As much as people can get detailed information and guidance specific to their situation online, that reduces the number of people that need to make a phone call to triage lines, GPs or other health providers, freeing up that capacity for those who really need to speak to someone and seek care.”
As you can see, many of the advances in telehealth come in the form of apps. Whether that’s building personalised healthcare plans through apps like Span or using digital health insurance through apps like Alan, a lot of healthcare services come easily packaged on a smartphone.
What Are The Gaps in Telemedicine?
As you can see, there are some gaps in telemedicine. One of the biggest is the one mentioned by Dr. Thiara – the NHS is often slow and limited by its funding. We’ll get to that later, but for now, let’s look at some of the reasons the public might be slow in adopting telemedicine-based healthcare delivery, pandemic notwithstanding.
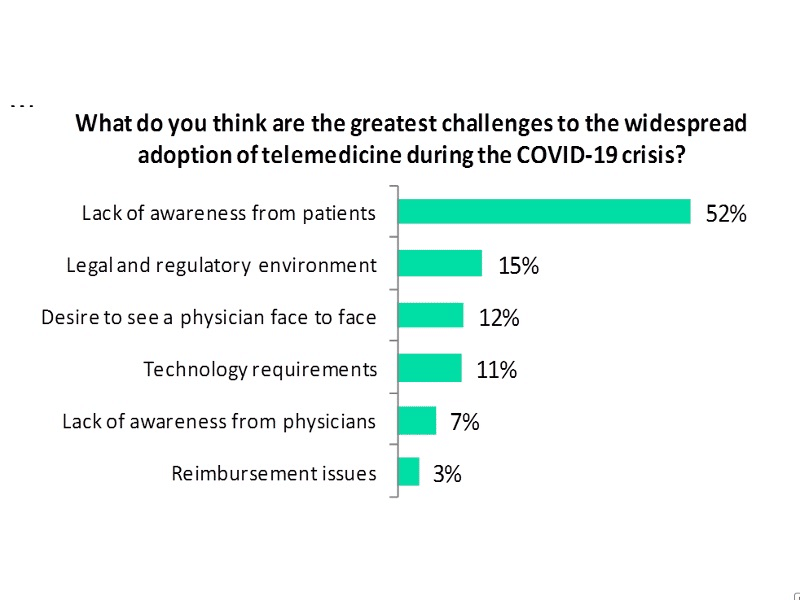
The above results are from the US, making it easy to discount the last category – reimbursement issues – though the cost of clinical services may well be prohibitive when it comes to private companies. One of the key reasons given is a lack of awareness from patients of the health outcomes telemedicine can support. The NHS has done a lot of work pushing its 111 services, and this has paid off. As their own data shows, this advertising led to an increase in calls.
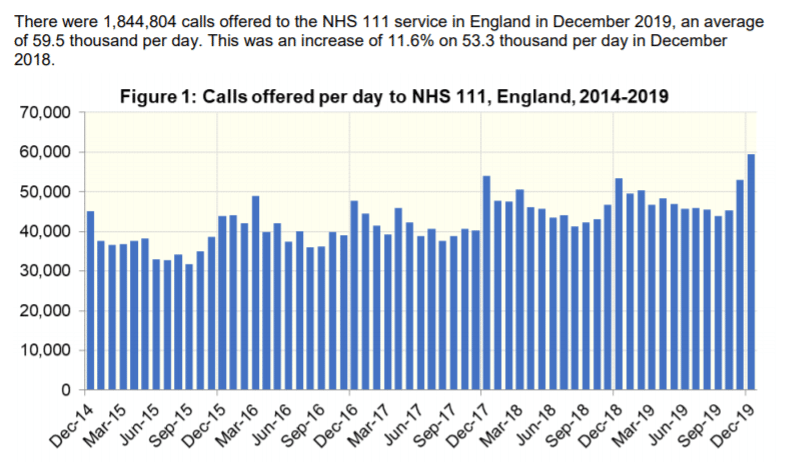
However, the NHS app isn’t anywhere near as well known. Though the work of NHS digital ambassadors looks set to change – between September and December 2019 the number of users has increased from 91,000 to 220,000.
The next barrier to adoption, the legal and regulatory environment, is a major challenge. Healthcare providers must be very careful with confidential information, and any telehealth services used must have sufficient security in place. In the United States, the requirements are enshrined in law in the shape of the HIPAA. Covid-19 has somewhat shifted the playing field here, with certain restrictions being temporarily lifted but there are concerns as to how this will be handled when the pandemic subsides.
Speaking to Healthcare IT News, Sam Shah, digital health advisor and former director of digital development at NHSX, shared his concerns. He stated that “In order for us to infringe those fundamental freedoms and protections, we should have a very good reason to do so. There might be a good reason to relax the rules for a period of time, however, there will come a point where COVID-19 will not be something we’re facing and, at that point, how are we going to clear up what’s left as a result of relaxing the rules now?”
This is particularly relevant for telehealth services that involve monitoring health – not everyone is comfortable with a private company having access to data on their blood pressure, mental health, or other factors that could affect insurance and employment. That includes health professionals, as well as patients.
The next two reasons for telehealth reticence – a desire to see a doctor face-to-face and information technology requirements – are not surprising. Many people will feel more comfortable discussing their health needs in-person with a familiar face, especially older patients or those with more complex needs.
It may well be that telemedicine isn’t suited for them – but that doesn’t mean it won’t benefit them. As Dr. Thakar points out “services like ours [Doctor Care Anywhere] can do much of the heavy lifting in cases that don’t require [physical assessment]. That’s at least 60-70% of primary care. So we can repurpose capacity and demand, so that those patients who most need to be seen in person, can be seen in person.”
The technology issue is something that applies on both sides – for healthcare practitioners and patients. As you can see below in Deloitte’s survey of US physicians, 35% of respondents noted their workplace doesn’t offer appropriate technologies, while 23% noted their patients weren’t interested or didn’t have the technology to support it.
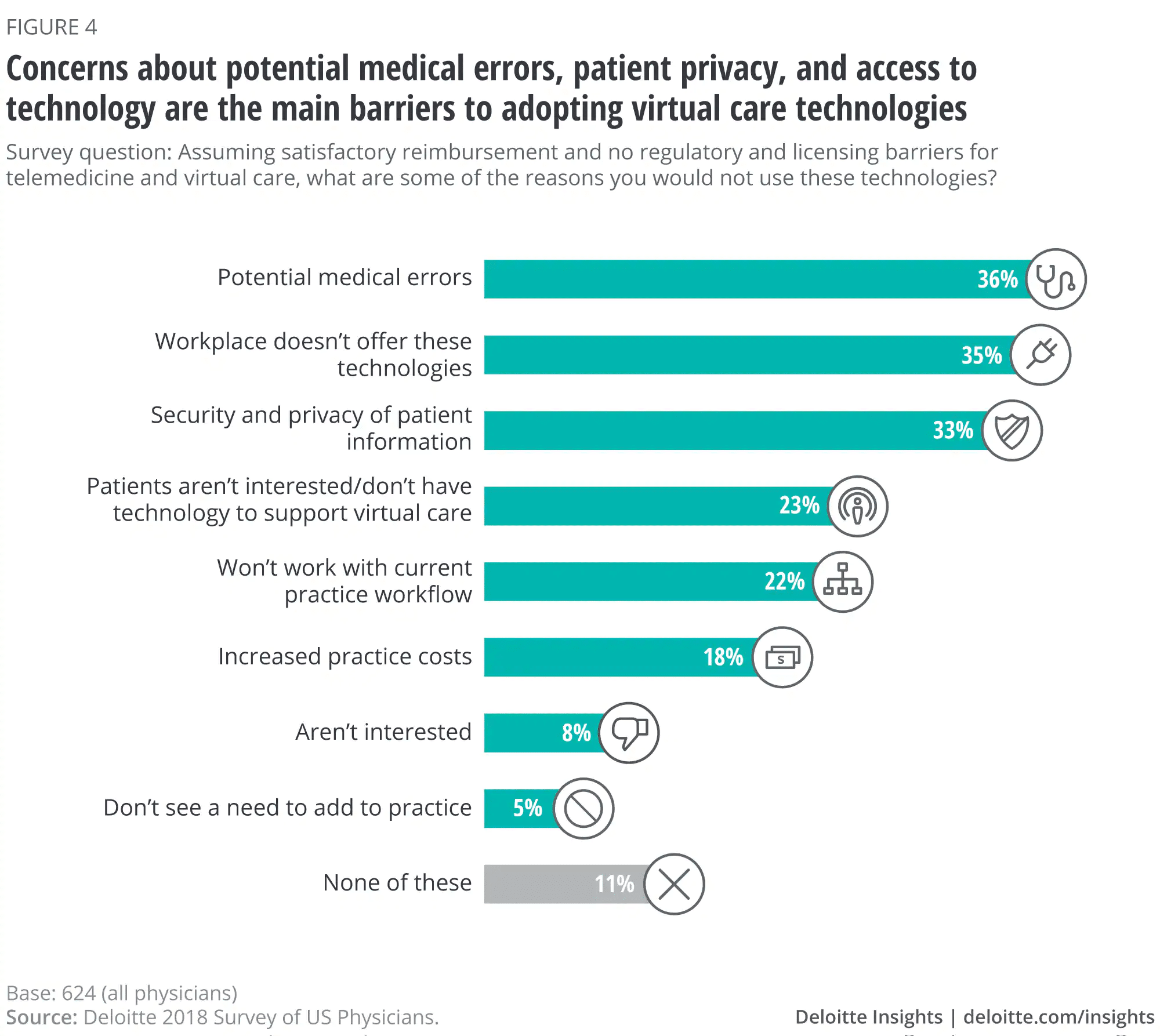
Telecommunications technology solutions like videoconferencing require a certain level of hardware, and many patients may not have regular access to this. There are lower-tech solutions – for instance, SMS telehealth has been used in places where people may not have internet access or smartphones, with great success.
Sam Shah notes that “if health services continue to digitise then there needs to be a reciprocal availability of internet for all, regardless of cost, so as not to limit access”, as well as pointing out that “Digitisation could be one of the ways we do that [address health inequality] but it needs support and funding.”
Regarding the accessibility of technology in public health services, the NHS has a long term plan which addresses some of this. Many NHS trusts don’t use a unified app, instead of having their needs split between numerous programs. Much of the plan involves investing in upgrading the telemedicine technology, making systems easier to develop, and interact with and using commercially available solutions that meet their stringent security needs rather than this piecemeal approach.
Companies like accuRx deployed their video consultation solutions quickly in response to Covid-19. Jacob Haddad, the founder of accuRx, told the BBC that they’d been “all hands on deck, getting features out” – and that they’d been fairly low-tech, designing solutions to suit what primary care physicians and patients would already have available.
Dr. Alexander Finlayson, who has worked on many global health projects, launched NYE Health. This software is designed to transform healthcare providers’ pre-owned technology to be NHS compliant, allowing them to make use of telehealth without having to upgrade their mobile devices or other hardware. With developments like this, this technological gap may well be the first to close.
What Does The Future Look Like For Telemedicine?
In general, the future of telemedicine – and telehealth in general – is looking bright. Forecasts suggest it will come out of the pandemic stronger than ever. This isn’t a surprise to many in the field. Speaking to CNBC, Dr. Mark Partner, a GP from the Cotswolds, said “It was always likely to happen, but not at this pace. Necessity is the mother of invention.”
With the increased adoption of telemedicine services, we can expect to see great benefits. Some of these are directly related to Covid-19. Gary Birks, general manager for UK and Ireland at Orion Health, told Healthcare IT News that their “intention is to reduce the inevitable burden that virus outbreaks can place on an already stretched health service. We want to alleviate spikes in demand.” Reducing the pressure on the NHS that is often overrun by the need to deliver urgent care is one temporary advantage, but there are long term ones, too.
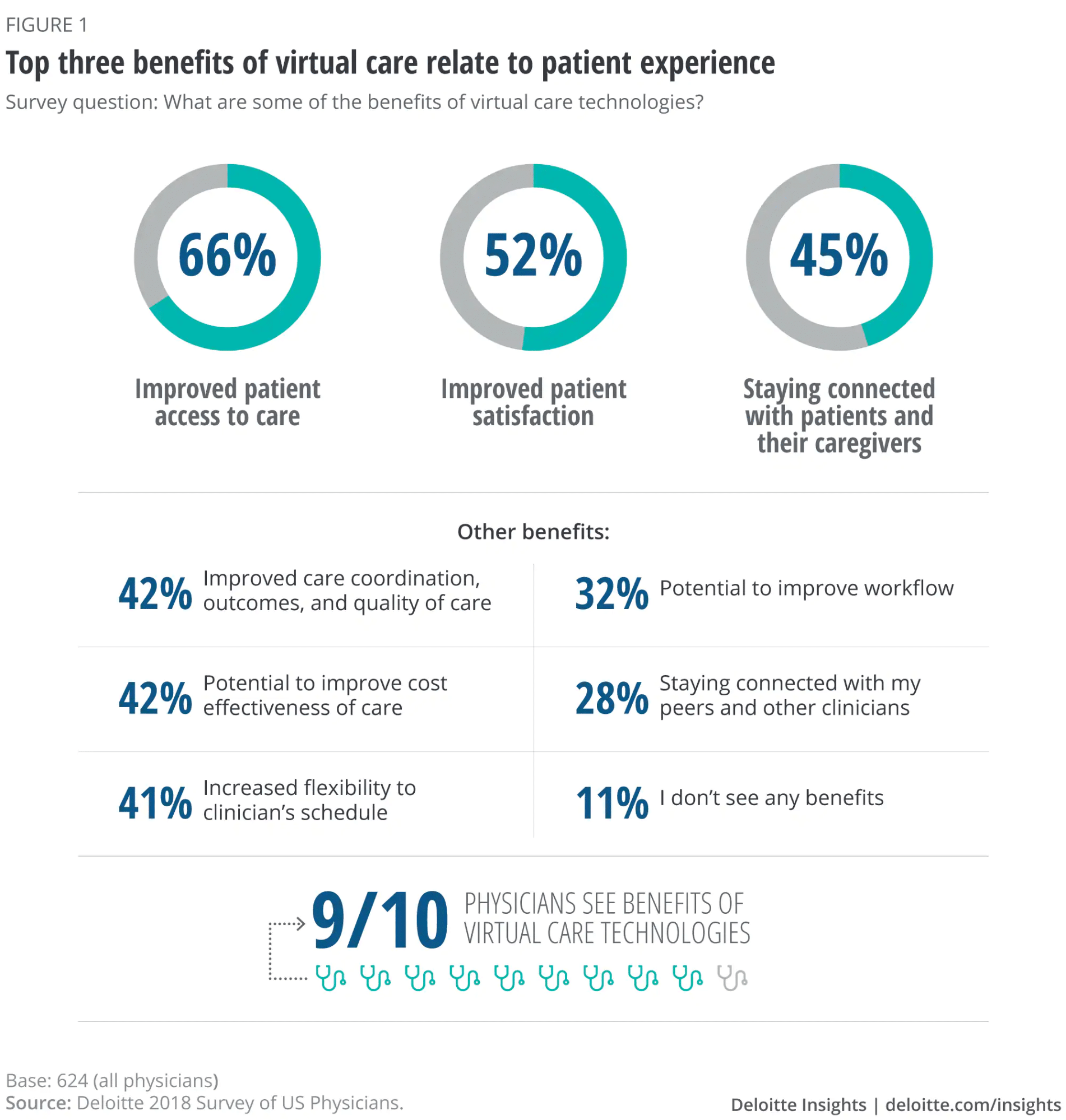
With the increased adoption of telemedicine, we should see improved access to care and an increase in connection between healthcare providers and patients. Not to mention a boost in general medical education. Dr Thakar wants to “make it so that patients and clinicians alike can avoid having to travel to and from clinics, wait in waiting rooms, then get a letter of the referral sent to them, all of that – if it’s what they want, and it’s medically appropriate.” He goes on to add that this can “can save a lot of time, money, and capacity for everyone involved.”
Being able to get great virtual care without physically travelling to a doctor’s office will make a huge difference in how healthcare works. Even for patients that do need physical appointments, there are telehealth technologies that can improve their experience. Dr. Thakar notes that even for complex patients, “collecting data and identifying trends, whether this is blood glucose or blood pressure…enables an improved evaluation of care which means doctors can make more informed decisions.” Monitoring apps and technologies, tracking all kinds of medical information from blood pressure to seizures, are likely to become more and more common – perhaps even available on prescription.
Finally, we should expect to see an increase in private health apps dedicated to overall well being rather than specific medical services, as people grow more able to manage their health digitally. Rachel Lett, the Head of Care at Span, told TechRound that “digital is hugely valuable to healthcare…[it] empowers people with ‘self-care’ and prevention of chronic conditions”. This self-management of health is liable to be one of the big drivers of the adoption of telehealth services.
Conclusion
While face-to-face consultations remain important, public trust in telemedicine and video visits has increased throughout the Covid-19 pandemic. It looks likely that the use of telemedicine services will continue even as the pandemic subsides, working alongside more traditional standard primary care services.
Many telemedicine founders and medical staff are optimistic about the future. Whilst there are hurdles such as strict regulation, the limited NHS budget, and access to technology, they all seem to be in agreement that digital transformation is inevitable, and likely to bring about positive changes to the healthcare field as a whole.
Get details on the security and trust built into RingCentral products and services.See NHS Professionals Case Study
Originally published Sep 17, 2020, updated Jan 17, 2023



