Telemedicine has its roots in the United States. It was originally designed to provide better medical care to rural communities. However, the benefits go beyond this and it’s slowly begun to be recognised worldwide. With the potential to save the NHS £7.5 billion, as well as an expected 27.7% compound annual growth rate (CAGR), it’s no wonder it’s a hot topic.
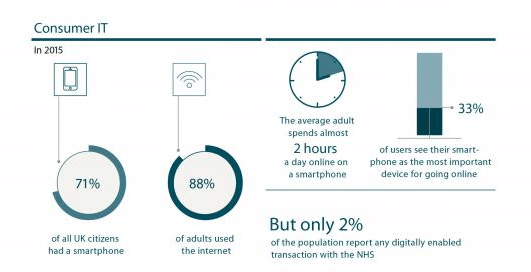
However, despite the majority of adults in the UK using the internet, only 2% of the population had undertaken a digitally enabled transaction with the NHS. Clearly, there’s a lot of room for telemedicine providers to move into the market – and with Covid-19 forcing the hands of many medical practices, now is the time.
What is Telemedicine?
Telemedicine is a small part of a wider field, known as telehealth. Whilst telehealth covers everything involving healthcare and technology, telemedicine is more focused. Specifically, it’s the digital provision of clinical services to patients. Telemedicine covers:
- Real-time consultations through text, phone calls, or video conferencing.
- Asynchronous (or store-to-forward) evaluations.
- Medical imaging being transmitted to specialists elsewhere.
- Prescriptions without in-person appointments.
Telemedicine and telehealth are sometimes used interchangeably – and there are a few things that are sometimes counted as telemedicine, and sometimes fit under the broader banner of telehealth. These are things like:
- Remote patient monitoring.
- Online therapy or rehabilitation appointments.
- Medical alert systems (usually considered to be its own field, telecare).
For simplicity, we’ll be using telemedicine to refer to the narrower definition, but may occasionally touch on other aspects of telehealth as many providers have a broad scope.
Introduction to Telemedicine Providers
Even with this narrower definition, there’s a variety of different telemedicine providers, all responsible for different services. Firstly, there are two kinds of ways these providers can work.
1. Provide to the NHS/private practices.
Some telemedicine providers provide their services to the NHS or private practices. This way they don’t need to provide the expertise of medical professionals, just the infrastructure. One of these telemedicine companies is medio.link. Their services include MDT rooms, virtual clinics, and a service that handles 40,000 calls a year between a Digital Nursing Hub and over 600 residential and nursing homes throughout the UK.
2. Provide direction to the public.
Alternatively, they can provide virtual care directly to patients. This usually comes in the form of apps, websites, or smart technology. However, it’s often still linked to the existing network of NHS and private doctors. One such example is Push Doctor, which links patients with available healthcare professionals. They provide a platform for patients to digitally connect with their GP and receive remote care after registering online through video consultations.
Broadly speaking, those are the main two categories of provider – those who interact only with healthcare providers, and those who interact with both healthcare providers and patients.
State of The Industry
The state of UK telemedicine is very different from the US. With the US, regulations vary by state, and healthcare services are impacted by what medicare will cover. This means that often, primary care can only be offered to people in certain locations (usually rural areas) or for certain reasons (if they’re elderly or unable to leave the house). However, the UK has a very different system.
Most people in the UK are registered with an NHS GP. Some people may also have private health insurance, or opt to go private for certain medical services. This means that any providers need to understand the NHS system and how to work either within or alongside it. It also means patients have certain expectations that they’ll expect to be met.
Of course, the big factor in this field at the moment is the impact of coronavirus. Many doctors have been forced to go remote purely because of the pandemic, and don’t necessarily have the infrastructure in place to support it. This forced acceleration into adopting virtual care platforms may well have a long term impact as more patients and professionals grow used to it.
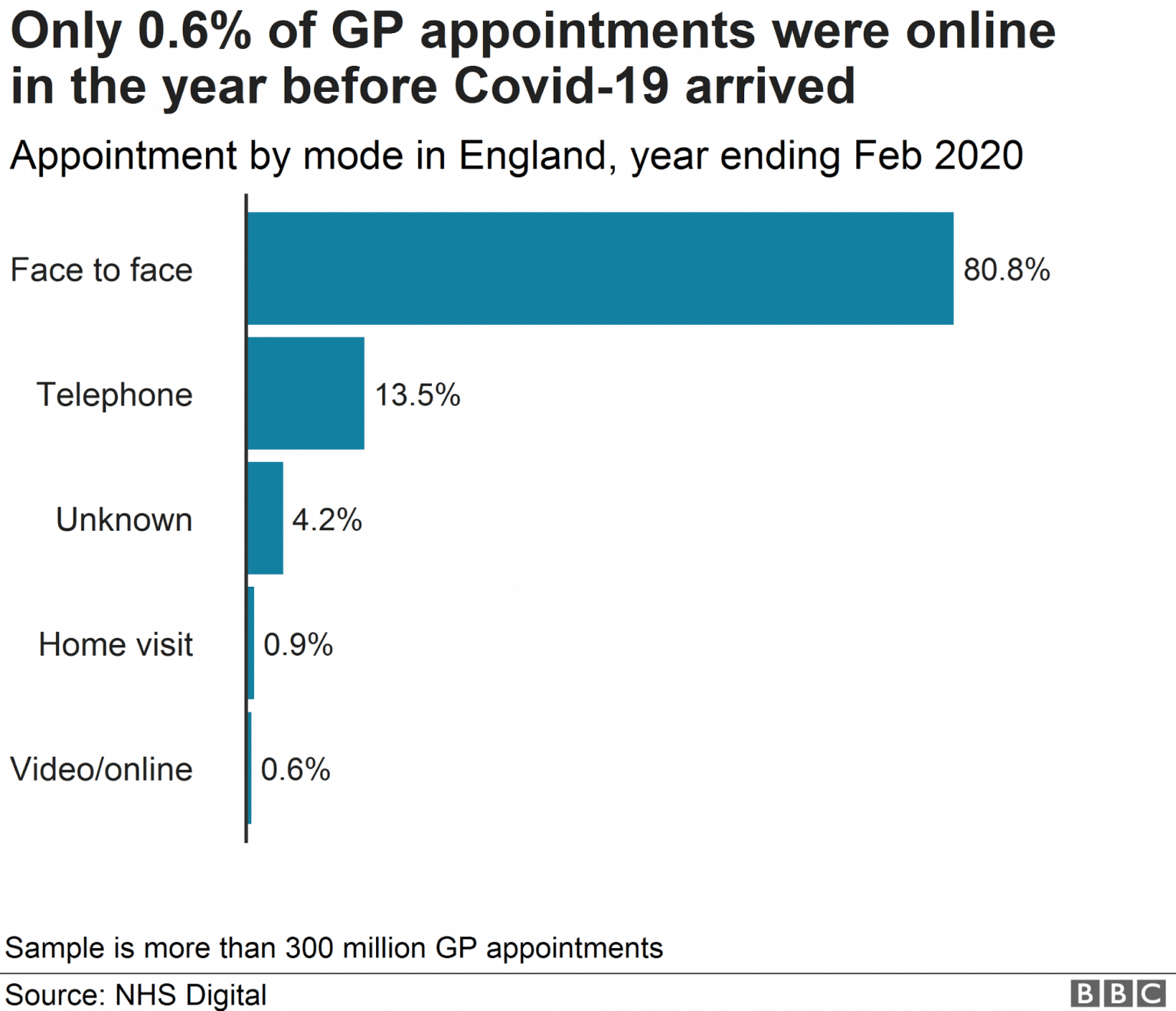
As you can see above, before February 2020 only 0.6% of appointments were online. However, according to the BBC, “GPs are seeing just seven in every 100 patients face-to-face because of the coronavirus outbreak” – meaning 93% of appointments are now online or via a phone call. Video visits are certainly new house calls.
One big question about the practicality of telehealth is can providers do telemedicine from home? Some telemedicine services focus on connecting patients to hubs – like medio.link’s digital nursing hub, or rural patients connecting to their local hospital. However, Covid-19 has led to a shift in this pattern, with remote consultations becoming the standard. With many GPs taking phone appointments from their homes, and only accepting in-person patients for urgent or more complex issues, it may well set a precedent for how virtual care will continue in the future.
Technology at Play
Telemedicine involves a lot of different types of technology. Some telemedicine companies focus on one specific aspect, others have a much broader scope. We’ll take a look at some of the main technologies at play in this field.
1. Video conferencing.
The main thing that people think of when they think of telemedicine services is the ‘doctor on-demand’ kind of idea – one where you can virtually see a doctor through your smartphone or computer as you need. For this to be effective, the video chat needs to be as high-quality as possible. It’s vital that any visual symptoms can be conveyed clearly – especially if the appointment is regarding something small, like a mole.
There’s also an added level of security needed, as the contents of the call need to remain confidential. Whilst in the US the concerns revolve around HIPAA, it’s not quite the same in the UK. The NHS has certain standards that need to be met, or exceeded, in order to be HSCN (Health and Social Care Network) compliant. However, in the midst of the Covid-19 crisis, there are some concessions being made.
The BMA (British Medical Association) states in their guidance: “Commercial products…can be considered where you urgently need to have a video consultation with a patient and if alternative channels are not available.” They go on to state that the risk of no consultation should be weighed against the risk of using these alternatives.
2. Phone consultations.
Not everyone has an internet connection capable of maintaining a video call, so phone calls remain a vital part of communication. Many practices have offered telephone appointments for some time – whether that’s for people who can’t physically access the practice or medication checkups that don’t require a physical assessment.
However, the way these have been done isn’t standardised between practices, and often involves a process very similar to in-person appointments. It often means calling up to book an appointment, being told a time period it will happen between, and then waiting to receive a call. This brings us on to our next relevant technology…
3. Scheduling software.
Telemedicine has the potential to move away from the conventional method of either phoning in to book through a receptionist or turning up and waiting between certain hours for reserved slots. Instead, by taking advantage of scheduling software, patients can book themselves into the diary.
Scheduling software displays which slots are available for the doctor you wish to see, and allows you to book in. This is similar to the technology used in other fields like booking hairdresser appointments. It can also be used to show you which doctors are available immediately, which is great for patients who aren’t looking for a particular practitioner and would just like a quick appointment or urgent care. It’s important to build in break times or accommodate longer appointments, as remote work can lead to burnout from those who aren’t used to it.
4. SMS reminders and results.
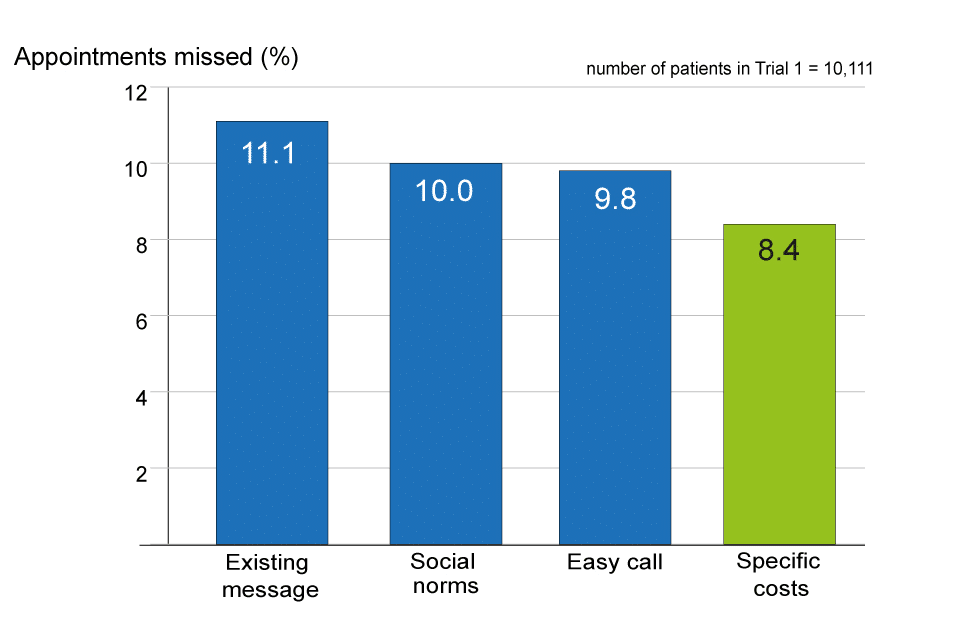
Rather than relying on emails and phone calls, more practices have moved towards SMS reminders. This is especially useful when used alongside scheduling software, as patients can leave the best phone number and opt-in to reminders. DNAs (did not attend) are a huge concern for many practices, and SMS reminders help reduce these. Currently, studies are being undertaken on the best phrasing for these reminders, with a mention of the associated cost seeming to be the best method.
SMS also provides a quick and easy way for people to receive test results. This has benefits for efficiency – people waiting on results don’t have to make time for a call – and security, as leaving a text message can be just as secure (if not more) as a voicemail.
5. Electronic prescriptions.
While there are already some systems in place for electronic prescriptions, they’re spotty and vary depending on your practice. Some pharmacies will only accept paper prescriptions, and some rely on you physically handing it in, rather than it being delivered to them.
Part of the difficulty of providing electronic prescriptions is that it requires buy-in from the pharmacies as well as the practices. Luckily, they’re becoming more common, and so are electronic pharmacies. Pharmacy2U is one great example of this, especially for repeat prescriptions. Patients can request the medication from the pharmacy, who requests it from the GP, who checks it over and then posts it out. Other pharmacies, such as Boots, have implemented similar services.
6. Secure store and forward capabilities.
Asynchronous consultations are incredibly important for a lot of patients, especially when it comes to ongoing conditions. They’re often used to pass information from the patient to the GP, and the GP to a specialist. For instance, a patient is experiencing a rash. The GP asked them to photograph it and send it through. Once they receive the photograph, they realise they don’t recognise it, and so they forward it to a dermatologist.
This would be incredibly difficult to schedule in real-time. Store and forward allows the patient to take the photograph in their own time, the GP to view it when they’re available, and the dermatologist to do the same. It also means that patients don’t have to spend time travelling to specialists unless they need a physical examination.
Due to the fact that it does contain confidential medical information, this has similar security requirements to video conferencing – with the added complication of storing the data.
7. Secure access to patient medical records.
Medical providers need to access patient records. Unless patients have opted out, their GP will have something known as a ‘summary care record’ (SCR), designed to avoid prescription errors and increase safety of care in other settings. This medical record includes (at least):
- Current medication
- Allergies
- Previous bad reactions to medication
- Name
- Address
- Date of birth
- NHS number
It can also include long-term conditions, important medical history, and notes about communication methods. The current situation means it also includes any Covid-19 based details like shielding and testing status.
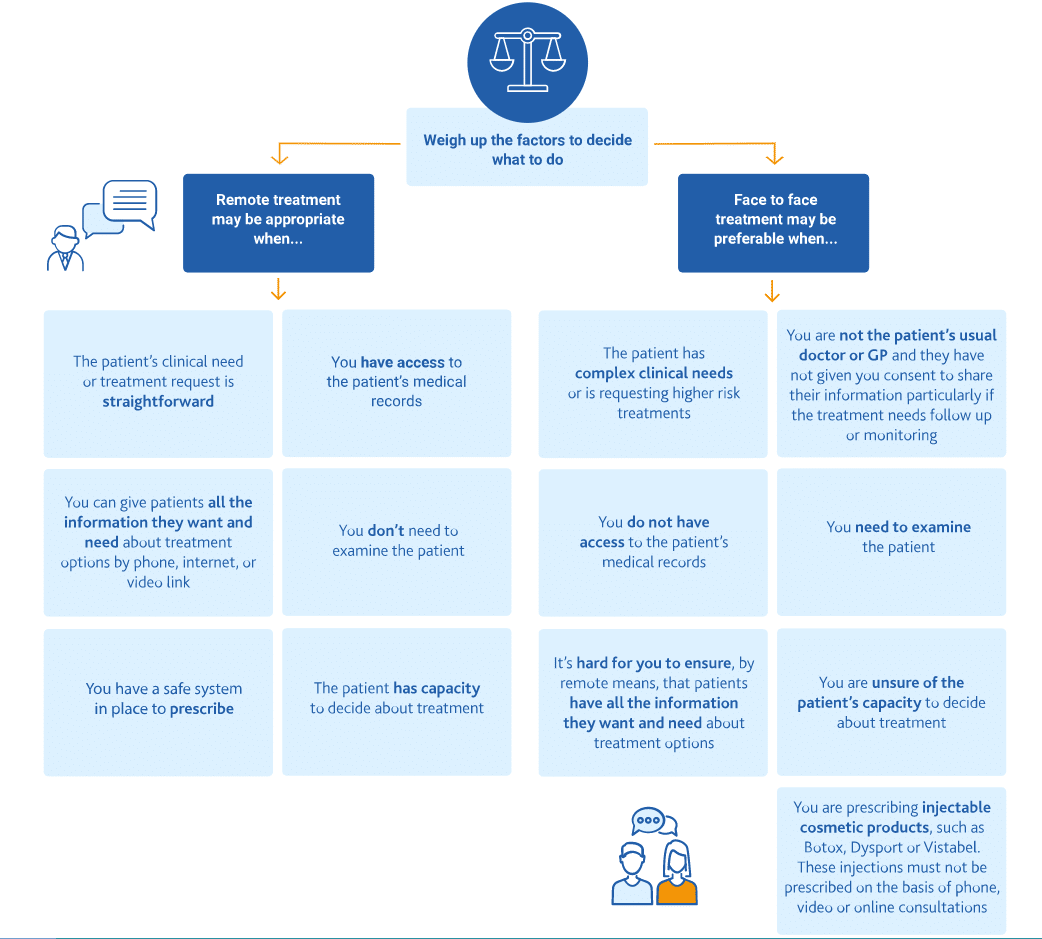
Telemedicine providers need to have secure access to at least the SCR and ideally full records in order to be able to provide care. For doctors and pharmacists working remotely, this means that those records must only be accessed securely and not stored. This is where VPN tokens, remote access, and other technologies come into play. The best telemedicine providers will be clear about how they access the data, how it’s stored, and what happens with it if you leave their care.
8. Machine learning for remote patient monitoring.
As mentioned earlier, sometimes remote patient monitoring falls under the general banner of telehealth, and sometimes it’s counted as telemedicine. We’ve included it here because it has some incredibly interesting technological links – in particular, the possible interactions with AI and machine learning.
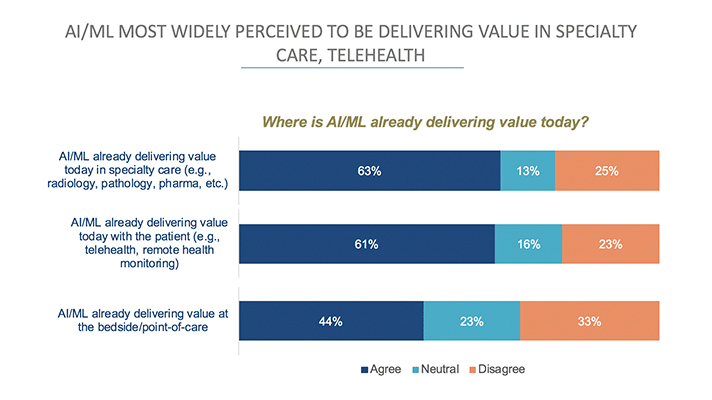
Remote patient monitoring usually involves one of two things – the gathered data being sent to the doctor directly to look through or being sent to a team to look for anomalies to flag up. However, machine learning has the potential to reduce this extra busywork by registering anomalies and alerting healthcare professionals. While this is a developing field – machine learning requires training from large datasets – it’s one that we should expect to grow quickly as AI capabilities improve.
Telemedicine Providers Who Are Disrupting The Industry
1. accuRx.
Originally focused on SMS messaging for healthcare providers, accuRx stepped up to help out during the Covid-19 pandemic. They built a video calling system quickly and provided it to clinics throughout the country. Thus allowing them to quickly open up online appointments.
The telehealth providers are trusted by 95% of NHS GP practices, which meant they could roll this out for free incredibly quickly. They also designed it to be able to work within pre-existing clinical systems, which makes it much easier to make use of. It’s even being used by specialists in the same hospital building, avoiding unnecessary contamination between departments.
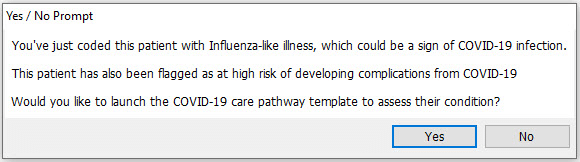
2. EMIS.
Emis offers a lot of different products, including a mobile version of their core telemedicine platform, EMIS web. EMIS web can be used to manage patients, schedule appointments, and generate detailed reports. One of the service provider’s case studies is Wingate Medical Centre in Liverpool, where the implementation of their software led to an increase in helping 40% more patients a day.
They’ve also provided a template of care for coronavirus, designed by medical professionals to improve the primary care pathways people access. This quick response to the emergent situation will likely encourage increased use of their software.
3.0TPP.
While accuRx and EMIS are designed for healthcare professionals, TPP provides a patient-facing app, Airmid. It’s designed to enable online appointment bookings, access to patient records, and order repeat medication. There’s also a web browser-based alternative patient portal, SystmOnline. When linked to their other software such as SystmOne, it provides a comprehensive solution to patient management and helps develop treatment plans.
SystemOne has been operational for around 20 years, meaning it has a lot of data. Their goal is to provide everyone in the healthcare system access to single shared Electronic Health Records (EHR), allowing for effective patient care. Since this can be accessed anywhere, it works well with telemedicine as it doesn’t rely on being based in a physical location.
4. Immedicare.
Born out of Airedale NHS Foundation Trust and Involve Visual Collaboration Ltd, Immedicare works specifically with care homes. They have a central digitally accessible hub that takes video calls from and stays in touch with care homes throughout the UK. The hub has a full clinical team with specialists from various fields, including emergency, community, and end of life care.
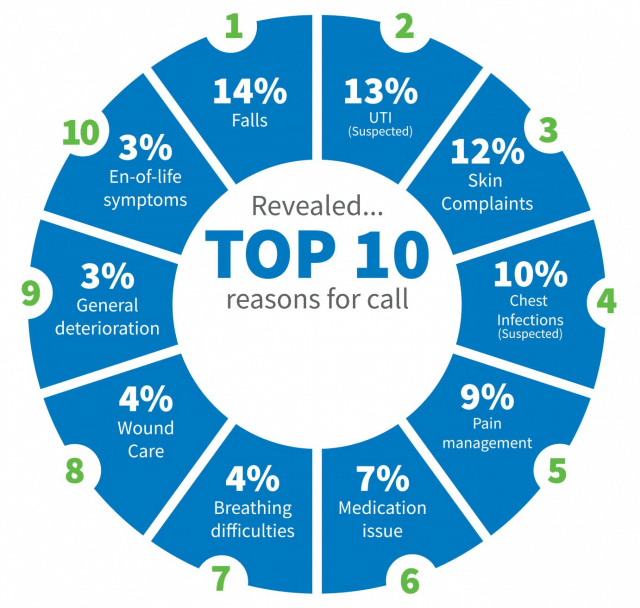
Immedicare aims to reduce A & E and GP visits for care home residents while providing the same level of healthcare. One of their case studies, Headingley Hall in Leeds, noted that in a single month they avoided 14 hospital admissions due to using these telehealth services. Such success could make a big difference to public health.
5. Push Doctor.
Another patient-facing app, Push Doctor provides video consultations between GPs and patients – their model is set up around the doctor on demand concept. In essence, virtual visits replace traditional appointments. They’re regulated by the Care Quality Commission and received the UK’s first ‘good’ rating in digital healthcare. They’re not designed as a replacement for a local GP, as patients remain registered with their local GP practice and can use Push Doctor alongside it.
However, Push Doctor is only available to patients whose GP practices have agreed to use it – potentially limiting how many people will have access to it.
6. GP at Hand.
GP at Hand, previously known as Babylon, is disrupting UK healthcare in a more unusual way than those above. In order to use it, you have to deregister from your local GP practice. This means moving your care entirely online to their teladocs, though they do provide physical assessments at certain locations in London and Birmingham. Their app also provides an AI-powered symptom checker, designed to triage without requiring human contact.
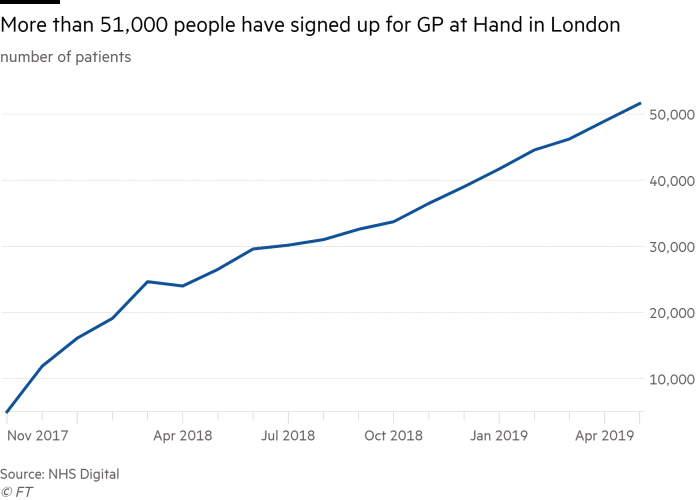
They currently have over 75,000 patients registered. That’s something which has raised a lot of questions for the NHS funding model, as they are based in one particular area despite being an online app. There’s a lot of debate over how this model may work in the future. This, combined with the way it was initially unclear that you had to leave your local GP and the extended registration time, has made it the centre of some controversy.
7. Skin Analytics.
Somewhere between telemedicine and the more general telehealth field is Skin Analytics. This is very different from the above, as it uses a custom-designed AI. They’ve partnered with some private healthcare providers – Vitality members can get skin check kits, and Superdrug is piloting an in-store checking service.
University Hospitals Birmingham NHS Foundation Trust (UHB) is working on a collaboration with them. This pilot study will involve patients capturing images of skin lesions, while AI technology triages them to determine which are safe and which need priority investigation by a dermatologist. Should this pilot prove successful, you can expect to see a widespread adaptation of this technology within the NHS.
The Future of Telemedicine
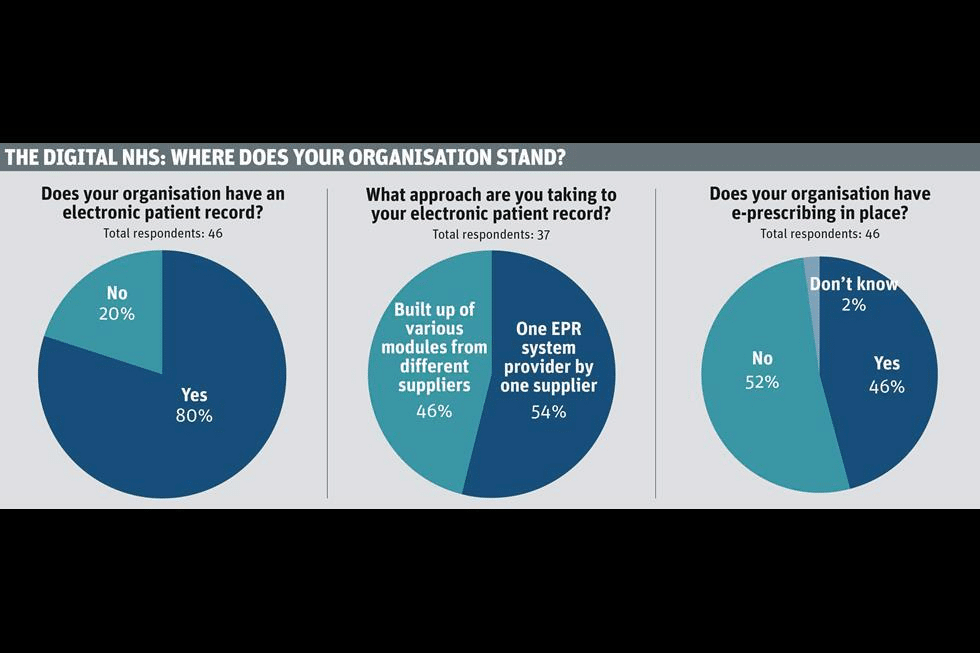
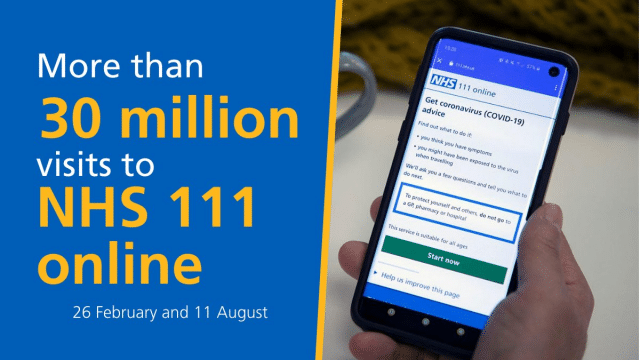
With Covid-19 showing that the answer to ‘can providers do telemedicine from home’ is a resounding yes, it looks like the adoption of telehealth services is set to grow. We know that over 96% of NHS GP practices have digital clinical record systems in place, meaning at a basic level the infrastructure is there to build upon. Patients seem willing to make use of telemedicine services, with the NHS 111 service having a huge volume of calls.
However, the slow implementation of telemedicine pre-coronavirus does show there’s a lot of work to be done. Implementing new technologies always comes with pushback, and sourcing funding, training, and simply time to adopt new methods may cause health professionals to tread more carefully.
Something that could hold back telemedicine is the hardware necessary to work remotely. Whether it’s VoIP phones, laptops, or even internet access, these are extra expenses that the NHS will need to find the money for – and this is where private practices may have the edge.
It seems likely that phone and video consultations will remain popular after the pandemic fades, along with more electronic pharmacies. The worry is that many will be content with this level, and won’t continue to push for new improvements. Luckily, pilot programs like UHB’s collaboration with Skin Analytics should provide peer-reviewed evidence as to the effectiveness of such technology, which should lead to increased investment.
Other aspects of telehealth may well also come to the fore. With apps like Calm and Betterhelp providing virtual therapeutic solutions, we may see an increased application of telepsychiatry in the field of mental health. Behavioral health issues or more complex mental disorders may still require in-patient treatment, but it’s possible online therapy services will become more common to deal with the shortage of local services. Equally, remote patient monitoring may reduce the need for regular clinical follow-up or check-ins for patients with chronic illness.
Conclusion
As it stands, telemedicine is on the cusp of being fully adopted. The coronavirus forcibly accelerated healthcare professionals into using it, and this could pay off with it continuing after the pandemic calms down.
The US has a much more varied healthcare map, with services differing between states and medicare provision. This means there’s a greater range of telehealth services available. Most services getting off the ground in the UK need to work within or alongside NHS provisions, which does put some restrictions on what they can do. This isn’t inherently a bad thing – it encourages a certain level of security and effectiveness – but it does mean the marketplace is different.
The real industry disruptors will be those who change the face of how diagnostics work – Skin Analytics DERM AI looks particularly promising here – or how registering for medical practices operates. With the ability to register with teledocs, it may well mean that local GPs become more focused on complex cases. Simpler appointments, meanwhile, like checkups or repeat prescription requests, move to an online hub.
Get details on the security and trust built into RingCentral products and services.See NHS Professionals Case Study
Originally published Sep 03, 2020, updated Jan 17, 2023



